| Refer A Friend |
 |
|
Thank you for showing your confidence in us through the referral of your friends! |
| Click to send a referral email |
| Quick Links |
Welcome !
In this issue of our newsletter:
Laser Therapy for Canker Sores, Cold Sores & Common Mouth Sores
From the American Dental Association
America's leading advocate for oral health
Overview
They are annoying and painful and there are plenty of things that can cause them – infections from bacteria, viruses or fungus; a loose orthodontic wire; a denture that doesn’t fit; or a sharp edge from a broken tooth or filling.
Mouth sores may be symptoms of a disease or disorder. A dentist should examine any mouth sore that lasts a week or longer. Among the most common mouth sores are:
Canker sores.(Aphthous Stomatitis) Small mouth ulcers with a white or gray base and a red border. Canker sores appear inside the mouth. They are not contagious. There may be only one canker sore or several and they can return frequently. Their exact cause is uncertain but some experts believe that immune system problems, bacteria or viruses may be involved.

Fatigue, stress or allergies can increase the likelihood of a canker sore. Some women may be more prone to them in their premenstrual cycle. A cut caused by biting the cheek or tongue, or reactions from hot foods or beverages may contribute to canker sore development. Intestinal problems, such as ulcerative colitis and Crohn’s disease, also seem to make some people more susceptible.
Treating Canker Sores: Laser treatments are the most effective, giving immediate pain relief and causing the ucler to heal in 24-72 hours. Also, they usually heal on their own after a week or two. Over-the-counter topical anesthetics and antimicrobial mouthrinses may provide temporary relief. Stay away from hot, spicy or acidic foods that can irritate the sore. See your dentist if the sores do not heal or are painful. Antibiotics from your dentist and some oral bandages can reduce secondary infection.
Cold sores. (Recurrent Herpes Labialis) Annoying and painful, cold sores, also called fever blisters, are groups of fluid-filled blisters. They often erupt around the lips and sometimes under the nose or around the chin. Cold sores are caused by the herpes simplex virus type 1 and are very contagious. The initial infection (primary herpes), which often occurs before adulthood, may be confused with a cold or flu and can cause painful lesions to erupt throughout the mouth.

Once a person is infected with primary herpes, the virus stays in the body and causes occasional attacks. Recurring cold sores look like multiple tiny fluid-filled blisters that most commonly appear around the edge of the lips. For some people, the virus remains inactive or dormant. For others, cold sores can follow a fever, sunburn, stress, emotional upsets or a break in the skin.
Treating cold sores: Laser treatments can give immediate pain relief and treatments can give immediate pain relief and the lesion will heal in 24-72 hours. Also, cold sore blisters usually heal in a week by themselves. Over-the-counter topical anesthetics can provide some relief. Your dentist may prescribe antiviral drugs to reduce these kinds of viral infections.
Leukoplakia.Thick, whitish-color patches that form on the inside of the cheeks, gums or tongue is known as leukoplakia. These patches are caused by excess cell growth and are common among tobacco users. They can result from irritations such as an ill-fitting denture or the habit of chewing on the inside of the cheek. Sometimes leukoplakia is associated with oral cancer. Your dentist may recommend a biopsy if the patch appears threatening.

Treating leukoplakia: The dentist examines the lesion and checks the biopsy results to help determine how to manage the disease. Treatment begins with removing the factors that contribute to the lesion: quitting tobacco or replacing ill-fitting dentures or bridges.
Candidiasis. This fungal infection (also called moniliasis or oral thrush) occurs when the yeast Candida albicans reproduce in large numbers. It is common among denture wearers and most often occurs in people who are very young, elderly, debilitated by diseases like diabetes or leukemia, or who have a problem with their immune system. People who have dry mouth syndrome are very susceptible to candidiasis. Candida may flourish after antibiotic treatment, which can decrease normal bacteria in the mouth.

Treating candidiasis: Control focuses on preventing or controlling the conditions that caused the outbreak. Good oral hygiene is essential. Clean dentures to remove Candida and remove the dentures at bedtime. Saliva substitutes and prescription medications may be helpful when the underlying cause of dry mouth is incurable or unavoidable.
For your better health!
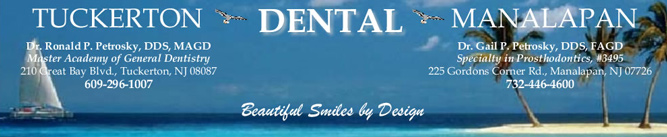
Tuckerton Dental
ph: 609-296-1007 - email: drpetrosky@comcast.net

